If Technologies Only Had a Heart
Nothing displays extra clearly the perfect engineering of the coronary heart than our possess unsuccessful attempts to imitate it. This background of the overall artificial heart is punctuated with the two good innovation and continual scientific failure. In 1962, John F. Kennedy challenged the scientific local community to land a gentleman on the moon and return him securely to Earth by the end of the 10 years. In 1964, cardiovascular surgeon Michael DeBakey persuaded President Lyndon B. Johnson to fund a software to acquire the 1st practical self-contained artificial heart, launching a race to efficiently make a person just before the moon landing. In 1969 each aims ended up seemingly obtained, with the Texas Coronary heart Institute implanting the to start with whole synthetic coronary heart just a few months prior to the launch of Apollo 11. On the other hand, while the moon landings have led to the Space Shuttle, Mars Rover, and Intercontinental Room Station, and (despite a very long lull) the latest aims to create a moonbase to deliver us to Mars, a trustworthy off-the-shelf whole artificial heart is nonetheless just out of attain.
At the outset, the synthetic coronary heart was aimed to be a life span replacement for the failing organ. This was a large bar to get to, since the very first style experienced an exterior compressor with an air line via the pores and skin into the patient’s entire body. Compressed air inflated and deflated Dacron pouches or sacs, which collapsed and expanded to displace blood from a encompassing sac. Although getting the compressor outside the house the entire body was practical, considering that the mechanical parts (which have been most prone to wear) could be very easily replaced, it would make for a bulky piece of tools to be wheeled about with the affected individual. It was difficult to see how this could be given to a client and expect them to dwell an even partly normal lifetime for many several years.
On the other hand, the background of the artificial heart is also intertwined with that of the coronary heart transplant. This was once more only a hopeful aspiration in the early 1960s, but by 1967 cardiac surgeon Christiaan Barnard in Capetown executed the first thriving transplant. Now, the intent of these initial synthetic hearts was improved. They did not want to be suited for a life span their intent was to keep the patient alive till a transplant donor could be identified. As with quite a few very experimental therapies, the to start with circumstance was finished on a affected person who had operate out of solutions. A 47-calendar year-outdated man was being operated on to fix a big aneurysm of the remaining ventricle that had thinned and swollen the coronary heart wall. He was staying supported by a heart-lung equipment, which bypassed the coronary heart and retained blood flowing through the overall body. Nevertheless, he could not be weaned from the device at the conclude of the procedure as his heart was too weak. He desperately desired a transplant. Denton Cooley, DeBakey’s affiliate, available him the new experimental whole artificial heart and he recognized. The individual was saved secure with the new machine for 64 hrs right up until a matching donor heart was discovered and then transplanted.
This seemed at initial a triumph for the overall synthetic coronary heart, but tragically the affected individual died 32 several hours later on from sepsis. Not only that but the system had broken each the blood and the kidneys, and the walls of the expandable sacs were coated with blood clots. This heralded a collection of issues that would keep on to thwart the scientists and engineers wrestling with this process. Infections and sepsis are a continuous problem to any gadget the place there is a wire that must permanently cross the skin. Products that move the blood will change its composition and the foreign surfaces will induce the blood to clot, ensuing in strokes and blood breakdown. The very first Jarvik heart, 1 of the subsequent iterations, was implanted in 5 sufferers and a person lived for 620 days. But two of the clients had serious strokes, and eventually all died of possibly sepsis or blood complications.
The research for a wholly implantable overall artificial heart carries on.
Heart transplantation also had a shaky get started, with Barnard’s first affected individual dying just after only 18 times. The first affected person in the United Kingdom, whose transplantation was performed by cardiothoracic surgeon Donald Ross at London’s Countrywide Coronary heart Medical center, survived for only 45 times, and the common achievements fee remained disappointing. The difficulty right here was not the mechanics of the operation or the preliminary efficiency of the new heart. It was the mismatch of the immune procedure of the recipient to that of the donor heart. Even though the donor coronary heart is matched as closely as possible to the patient with the key tissue sorts, the immune system should be suppressed to end the heart getting rejected. Medicines to suppress the immune program have been not very innovative in the early times, but the improvement of ciclosporin in the early 1980s generated a revolution in immunosuppression that significantly enhanced the good results of heart transplantation. Now, it is a sufferer of its possess achievement, with lots of much more individuals in will need of a transplant than there are donors. Only about 200 transplants are carried out in the U.K. every single year even with far more than 750,000 living with heart failure, and equivalent figures are witnessed throughout the world. To fill this hole, researchers have been genetically modifying pigs to make their hearts appropriate with the human immune program so that they can be transplanted to individuals devoid of staying turned down. This has proved quite complicated and demanding, but initial clinical transplants began in 2022.
The achievement of heart transplantation, however, had reinvigorated the lookup for the overall synthetic coronary heart, with the extra achievable target of retaining the client alive until eventually a donor is observed, or “bridge to transplant” as it is called. For a long time, the synthetic coronary heart technologies have enhanced by way of adjustments to extra biocompatible elements, far better valve structure, and more effective handling of blood flow. Successes have been accomplished: one particular research saw 80 percent of people on the artificial hearts surviving for around a yr, and some for 6 years. The longest time a affected individual was supported to transplant was 1,373 times. But critical infectious complications have been even now widespread, and the goal of a complete “destination” treatment for artificial hearts was however a distant desire.
Meanwhile, the urgent will need to bridge to transplant had taken the know-how in a different direction. Alternatively than replacing the failing coronary heart wholly, the plan was to assist it by aiding the blood flow. The ventricular aid product, or VAD, took blood out of the ventricle of the heart by a entirely distinct route and pushed it into the aorta at superior pressure. This added to the blood becoming ejected from the heart and thereby magnified the effective cardiac output. It also solved yet another issue encountered by the engineers of overall artificial hearts—how to balance the ideal and still left heart-blood flow. The amount of blood circulating in the remaining ventricle/entire body loop must be really near to that in the suitable ventricle/lung loop. With 100,000 beats a day, even a teaspoon of difference at each individual conquer would include up to 500 liters of blood in the mistaken spot. The heart has developed complex biological mechanisms to make absolutely sure this does not transpire, but the engineers ended up possessing huge battles to attempt to do the exact same with responses units. For VADs, either the suitable (or a lot more ordinarily) the left ventricle can be independently supported, having this problem away.
The longest time a affected person was supported to transplant was 1,373 days.
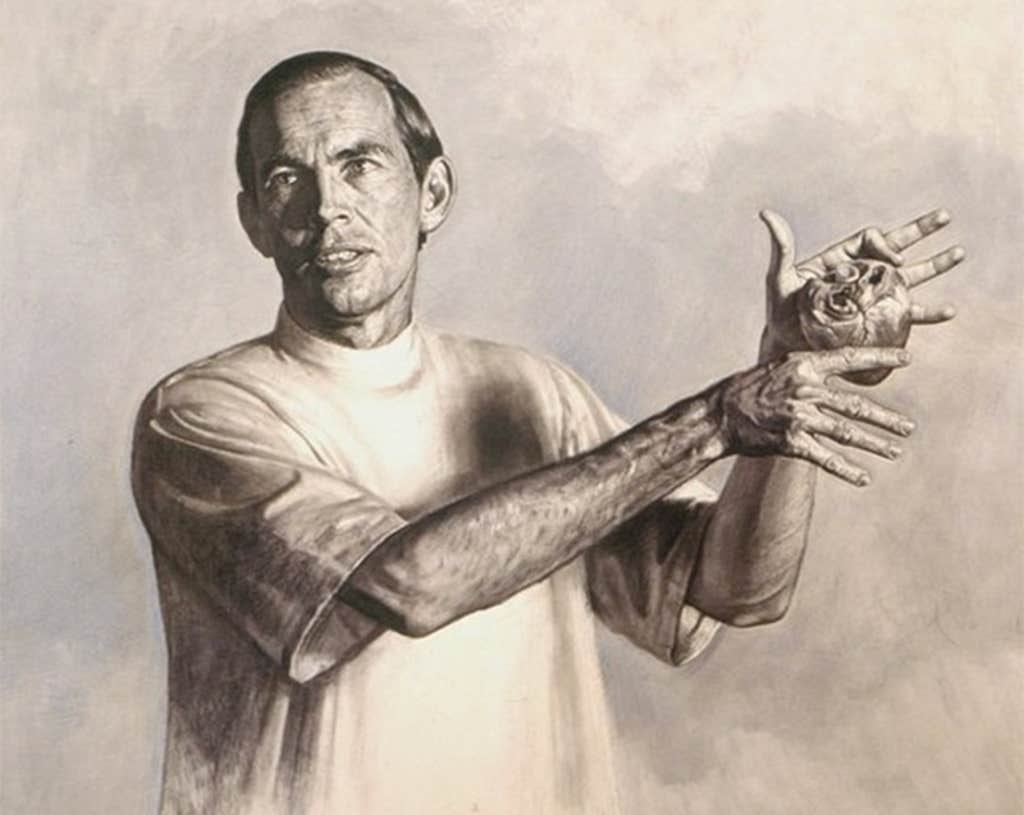
Left ventricular help equipment, or LVADs, have produced a revolution in treatment for finish-stage coronary heart failure. Additional than 15,000 LVADs have now been implanted globally, and close to a 3rd of people with close-stage coronary heart failure are now supported on LVADs. The intention is commonly to bridge the patients to transplant, but in actuality the scarcity of donor hearts indicates that sufferers can normally keep on LVAD help for many years. Survival prices of in excess of 50 p.c are seen at 7 several years, and there are stories of people dwelling up to 13 decades on these products. LVADs have therefore come to be by default a remedy in on their own. Again, technological know-how has progressed, with newer LVADs executing better. A breakthrough strategy was to quit imitating the heart, with its pulsing motion, and go to regular movement of blood. Rotating paddles (impellers) force the blood along in a continuous motion, generating a sleek unbroken stream. This has the curious side outcome of developing a patient without the need of a pulse, which can be disconcerting for the unsuspecting doctor as nicely as making some unwelcome side results as the human body adapts to the new circulation. Exterior battery packs are continue to an inconvenience and a source of an infection, but techniques are staying designed that transfer energy transcutaneously (throughout the pores and skin) based mostly on induction (like domestic induction stoves). The LVAD models would even now want a modest, implanted battery in scenario of a short-term product failure—and it has been regarded for external battery packs to be snatched from clients by purse robbers!
The research for a absolutely implantable complete synthetic heart continues. Attempting to create external transcutaneous models to entirely energy the calls for of the heart is the largest barrier. Specs for a overall artificial coronary heart involve it to pump eight liters for each minute of blood in opposition to a blood tension of 110 mmHg. (The biological ability storage molecule adenosine triphosphate [ATP] would be necessary in portions larger than 50 % your system body weight per day to electricity your very own coronary heart to do that, if ATP have been not constantly renewed in cells.) Compressors have been miniaturized to be extra moveable, but it has been a battle to make them absolutely implantable. Below it seems that the VAD technological know-how could maintain a alternative, dispensing with compressors completely and applying alternatively the impeller devices, with twin right and left VAD doing work alongside one another.
Options appear tantalizingly shut, but no one is anticipating an quick experience. The several failures more than the yrs have certainly generated in researchers a humility and awe for the pure engineering of the coronary heart. ![]()
Sian E. Harding, a regarded authority in cardiac science, is Emeritus Professor of Cardiac Pharmacology in the Countrywide Heart and Lung Institute at Imperial School London, where she led the Division of Cardiovascular Sciences and the BHF Centre for Cardiac Regeneration. She is the writer of The Beautiful Equipment, from which this write-up is excerpted.
Direct image: Jackie Niam / Shutterstock